our promise
We strive to build and establish enduring, supportive relationships with those in the autosomal dominant hypocalcemia type 1 (ADH1) and hypoparathyroidism communities. We commit to approaching these relationships with honesty, integrity, and transparency. We respect the independence of patient organizations, and we actively seek to include the unique perspective of patients, families, and advocates in the drug development process by listening to and learning from them.

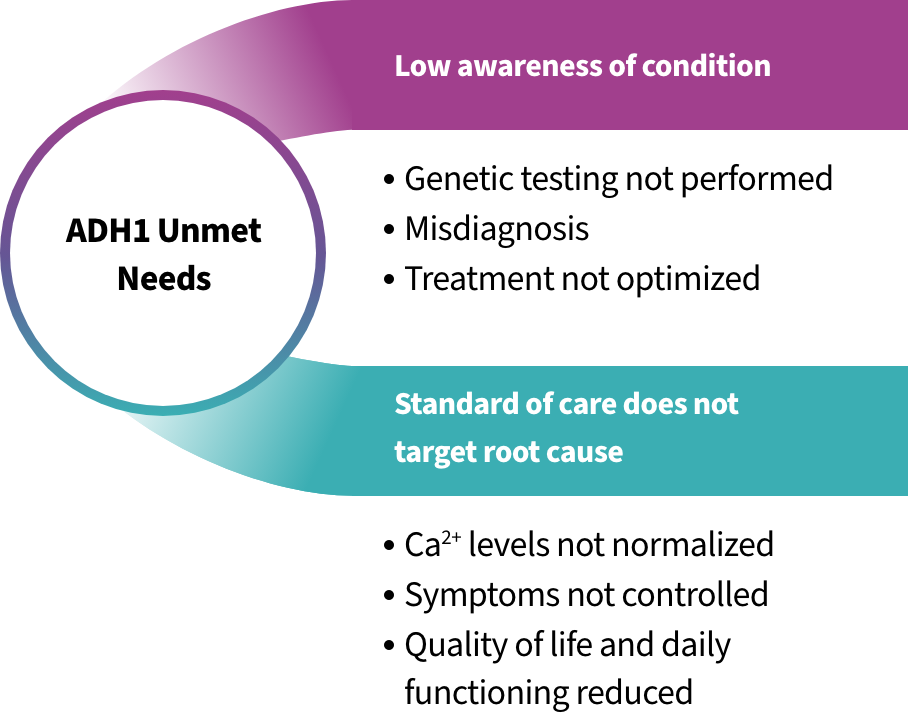
we understand the unmet needs of those living with ADH1
Current standard of care for people with ADH1 (calcium and vitamin D supplementation) may cause calcium levels in the urine to become too high (hypercalciuria), leading to kidney complications. To reduce this risk, a common treatment goal is to maintain blood calcium levels at the low end of the normal range or slightly below it.1 As a result, many people with ADH1 continue to have symptoms associated with low blood calcium (hypocalcemia) that impact their daily function and overall quality of life.2,3
ADH1 is often misdiagnosed as chronic hypoparathyroidism or idiopathic hypocalcemia.1 Some people with ADH1 never learn of the underlying genetic cause of their condition and may never receive optimal management. Given the potentially serious clinical features of ADH1, it is important to determine when genetic testing may be appropriate for people with nonsurgical hypoparathyroidism.1,2
ADH1 patient resources
BridgeBio actively seeks to include the perspectives of patients, families, and advocates in our drug development process. This partnership and collaboration are essential for understanding what the community finds meaningful in new treatment options and the gaps in current care. Connect with our patient advocacy team at [email protected].
HypoPARAthyroidism Association
Patient advocacy organization committed to providing education and support for individuals affected by hypoparathyroidism.
Visit siteHormone Health Network
Patient resource provided by the Endocrine Society focusing on hypoparathyroidism education.
Visit siteNational Institutes of Health (NIH)
Provides information on hypoparathyroidism causes, symptoms, treatment, clinical studies, and additional patient resources.
Visit siteMedlinePlus — National Library of Medicine
Patient resource providing information on the causes, symptoms, tests, and treatment of hypoparathyroidism.
Visit siteADH1 patient stories
-

meet Alexis
Alexis is a determined wife, mother, and self-proclaimed “social butterfly” who has been living with ADH1 for more than 25 years. She had her first seizure at 6 months old, which led to a hospital visit and diagnosis of hypoparathyroidism. Her childhood included multiple hospital stays due to violent muscle spasms and loss of consciousness during seizures.
Although the seizures stopped when she was 12 years old, Alexis continued to experience high blood pressure and calcification of her kidneys. At 16, she received a genetic ADH1 diagnosis after countless doctor visits, tests, and treatments.
“I lived in the hospitals… I regularly went into the hospital from 6 months old all the way up until I was 11.”
 Despite her ADH1 diagnosis, Alexis has always remained outgoing and determined to pursue her passions. Hypoparathyroidism caused her to fatigue easily, but she pushed herself and became a cheerleader in high school. She developed learning disabilities due to her frequent childhood seizures but met with a tutor every morning to succeed in her education.
Despite her ADH1 diagnosis, Alexis has always remained outgoing and determined to pursue her passions. Hypoparathyroidism caused her to fatigue easily, but she pushed herself and became a cheerleader in high school. She developed learning disabilities due to her frequent childhood seizures but met with a tutor every morning to succeed in her education.
“I still did it even though there were days I couldn’t get out of bed. I craved that, wanting to be a kid. I was still hurting. But I had to hold on to hope. I had to keep going.”Although told by many doctors that she would never become a mother, Alexis and her husband have two young sons – Jackson and Joseph. Throughout her pregnancies, Alexis dealt with fears of her own mortality and of her children inheriting the gene variant that causes ADH1.
“When I was told I was pregnant with Jackson, I was terrified because all I’ve heard was, ‘You’ll die if you ever have kids.’ I was so scared. And it took [my doctor] to say, ‘Alexis, it will be okay.’”
Alexis continues to live in pain, but she remains resolute. She wants people to know that although the consequences of ADH1 can be challenging, there is always hope.
“I have pain every day – it feels like I have arthritis in my whole body. I get kidney pain all the time. But I’m able to live with it. It’s hard to keep going… but there are ways to help.”
-

meet Jackson
Jackson underwent genetic testing for ADH1 at birth, since his mother Alexis was diagnosed with the condition after years of unexplained seizures and eventual chronic kidney disease. The results revealed that he had inherited this rare condition.
Alexis worried that her son would experience the same arduous medical treatments, frequent hospital stays, and feelings of alienation that she did as a child. Fortunately, due to advancements in medical knowledge, Jackson’s experience with ADH1 has been less difficult than his mother’s.
 Jackson likes to run and play outside with his friends and younger brother but faces significant challenges that most children do not face. He fatigues quickly and experiences body pains, but he tenaciously keeps going. Although his experience has not been as debilitating as his mother’s, he too has experienced seizures caused by low calcium levels. He doesn’t enjoy taking medicine every day and recognizes that it’s difficult for other children to understand his condition.
Jackson likes to run and play outside with his friends and younger brother but faces significant challenges that most children do not face. He fatigues quickly and experiences body pains, but he tenaciously keeps going. Although his experience has not been as debilitating as his mother’s, he too has experienced seizures caused by low calcium levels. He doesn’t enjoy taking medicine every day and recognizes that it’s difficult for other children to understand his condition.“He has moments where he says, ‘I wish I didn’t have to do this,’” Alexis explained.
Alexis guides her son with compassion, empathy, and faith in their combined strength to keep pushing forward. She wants other parents of children with ADH1 to know that they should not lose hope.
“Even if there’s no cure, you can still live your life.”
References
- Roszko KL, et al. Autosomal Dominant Hypocalcemia Type 1: A Systematic Review. J Bone Miner Res. 2022;37(10):1926 – 1935.
- Mannstadt M, et al. Hypoparathyroidism: Genetics and Diagnosis. J Bone Miner Res. 2022;37(12):2615 – 2629.
- Roszko KL, et al. PTH 1-34 Replacement Therapy Has Minimal Effect on Quality of Life in Patients With Hypoparathyroidism. J Bone Miner Res. 2022;37(1):68 – 77.